Morton Plant Hospital's Structural Heart Clinic Adapts to Serve Patients During Pandemic
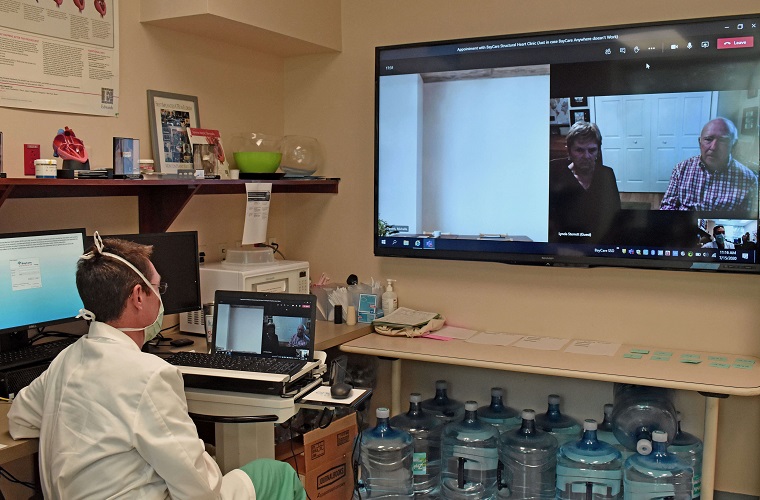
Sitting in their home in St. Simons Island, Ga., and staring at a screen on a random Wednesday afternoon, Jack and Lynda Sterrett weren’t just watching television or checking email. They were "at" Jack's follow-up appointment with Joshua Rovin, MD, FACS, Cardiovascular Surgeon and Medical Director, Center for Advanced Valve and Structural Heart Care at Morton Plant Hospital.
Rewind the clock a few months and this follow up would have been in-person at the structural heart clinic. Though some primary care visits were happening via telemedicine, heart patients typically were seen in-person. Then came COVID-19, changing business as usual around the world and here at Morton Plant Hospital.
Though most transcatheter aortic valve replacement (TAVR) surgeries, like Jack's, were delayed in March when BayCare postponed elective surgeries, the need to evaluate and possibly treat patients did not disappear. Heart issues did not go away, and some needed immediate treatment.
When BayCare offered physicians the telemedicine option, the structural heart team didn’t hesitate. They recognized the opportunity this presented to offer patients the care they needed while keeping them safe during a pandemic.
Within a day, the team was seeing patients using BayCareAnywhere®, a telemedicine healthcare app that individuals can download to a smartphone or tablet.
Patients and families who would have been in the office were now on a large screen while a cardiologist, a surgeon and a nurse practitioner sat together discussing the patient’s condition and medical history. While many structural heart clinics across the nation closed in April, telemedicine allowed Morton Plant’s clinic to continue meeting the needs of its patients. In April, the clinic saw more than 90 percent of its patients using telemedicine.
Being out in front is nothing new to Morton Plant’s structural heart team. They brought TAVR surgery to the Tampa Bay area in 2012, and in the ensuing years, the team has performed more than 1,500 surgeries while keeping abreast of the latest breakthroughs to ensure each patient has the best hope for a successful outcome.
While telemedicine may seem minor compared to the complex surgeries that have been performed and medical strides that have been made, the team recognized that a successful outcome had to start with an initial visit that kept the patient comfortable and safe.
"Technology gave us the opportunity to continue to provide our experience and expertise to help individuals with heart valve disease even during a worldwide pandemic," said Rovin.
Not only did the team consider patient safety when offering telemedicine, but it also made patient satisfaction a priority. The clinical team, of the structural heart program, creates a BayCareAnywhere® account for patients and sends them an email with all their information. The patient simply opens the email and clicks the link. Someone on the team also calls the patient to walk through the process and offers to do a test call if it makes the patient more comfortable.
"We can use telemedicine to see patients for all appointments except the one closest to the surgery," said John Ofenloch, MD, cardiovascular surgeon and chief of cardiothoracic surgery at Morton Plant Hospital. "This help provide a level of comfort for many patients."
While all patients, unless otherwise requested, continue to have a one-week follow-up appointment via telemedicine, most patients have resumed coming in-person for the initial consultation. That doesn’t necessarily mean less use of telemedicine as the team continues to find new ways to use technology to satisfy patients.
Many patients want more than one family member to participate in the consultation, but guidelines from the Centers for Disease Control and Prevention only allow one visitor with the patient. The team has begun to bring the additional family members into the visit virtually. They can see the clinicians in the examination room, ask questions and offer information to help the doctors make a better decision.
Putting the patient’s needs first has always been one of the driving forces of those who are a part of the Structural Heart Clinic.
“From the outset, we have stuck to a multi-disciplinary approach with a cardiologist, a heart surgeon and one or two nurse practitioners working as a team to assess each patient,” said Rovin. “Then, the surgeons and cardiologists meet weekly to discuss each case and decide the best option for the patient.”
Technology has begun to play into this as well. If someone cannot be at the team meeting in person, they can join via Microsoft Teams, adding additional knowledge and experience to each patient review.
“The benefit of our team is that the cardiologist and doctor who saw the patient will present the case to the other 10 people on the team to get everyone’s opinion,” said Michael Kayatta, MD, cardio thoracic surgeon and member of the Morton Plant Hospital Valve Clinic Team.
Many may think the use of telemedicine means a less personal approach, but patients at Morton Plant Hospital’s Center for Advanced Valve and Structural Heart Care would disagree.
Just ask Jack. Originally scheduled for April 1, his TAVR had to be postponed until May 5 because of the halt to elective surgeries. “They called weekly to check on me and everything was perfect,” he said. He reported he had almost no recovery. He spent eight days total in Florida, and within a week of returning to Georgia, he was back to walking three miles each day.
Speaking up on the screen in the office, he told his team, “You guys have been wonderful. Thank you.”